🧠
1. Magnusson et al. (2010) – The Pathogenesis of Tendinopathy: Balancing the Response to Loading
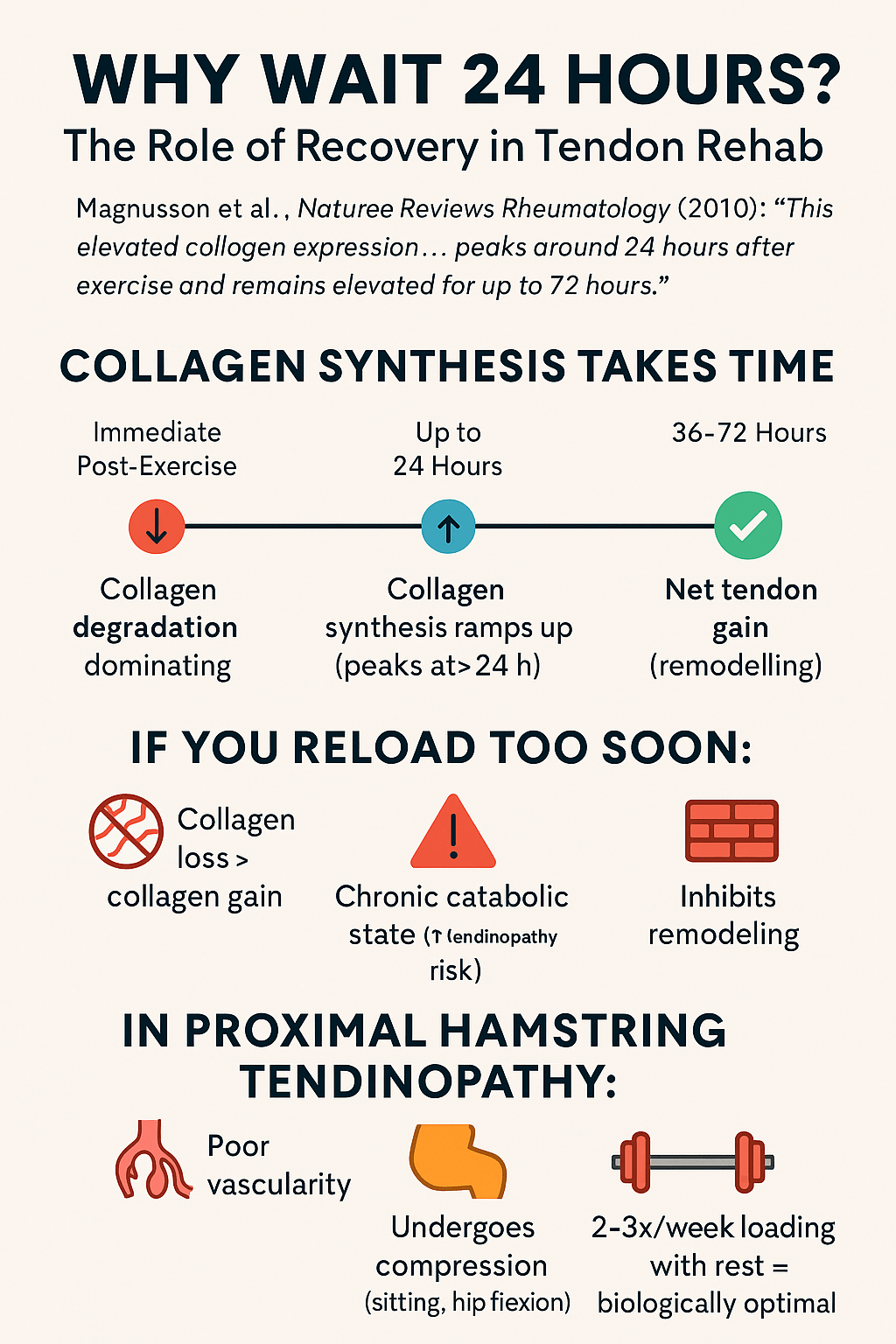
- Tendon tissue is metabolically active and adapts to both loading and unloading through collagen synthesis and degradation cycles.
- Collagen synthesis peaks ~24 hours post-exercise and remains elevated for up to 72 hours, while collagen degradation peaks earlier—underscoring the need for recovery time.
- Overloading can lead to pathological changes, such as disorganized collagen, increased proteoglycans, hypervascularity, and tenocyte rounding.
- Tendinopathy does not feature classical inflammation but is marked by cellular apoptosis, increased MMPs, and altered ECM signaling.
- Fibroblasts (tenocytes) act as mechanosensors in tendon remodeling and produce key ECM proteins in response to strain.
- Too little or too much mechanical loading disrupts the balance of tendon remodeling and may initiate degenerative changes or fail to stimulate adaptation.
🧩
2. Couppé et al. (2015) – Eccentric vs. Concentric Exercises in Tendinopathy
- No strong evidence supports superiority of eccentric over concentric exercise for tendinopathy—benefits likely stem from mechanical load, not contraction type.
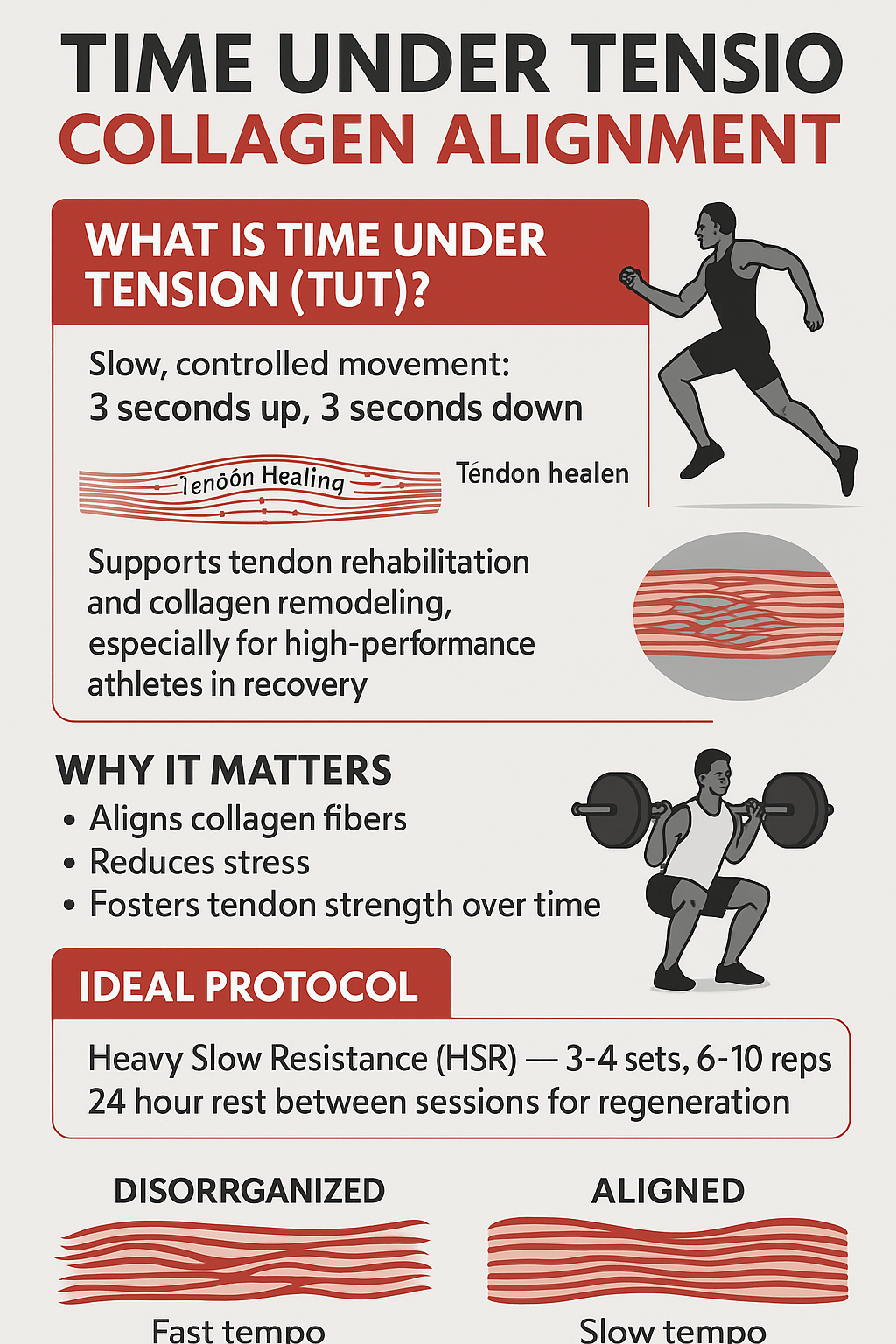
- Tendon fibroblasts are strain-sensitive, with optimal collagen response observed between 3–5% strain (e.g. ~90% MVC loading).
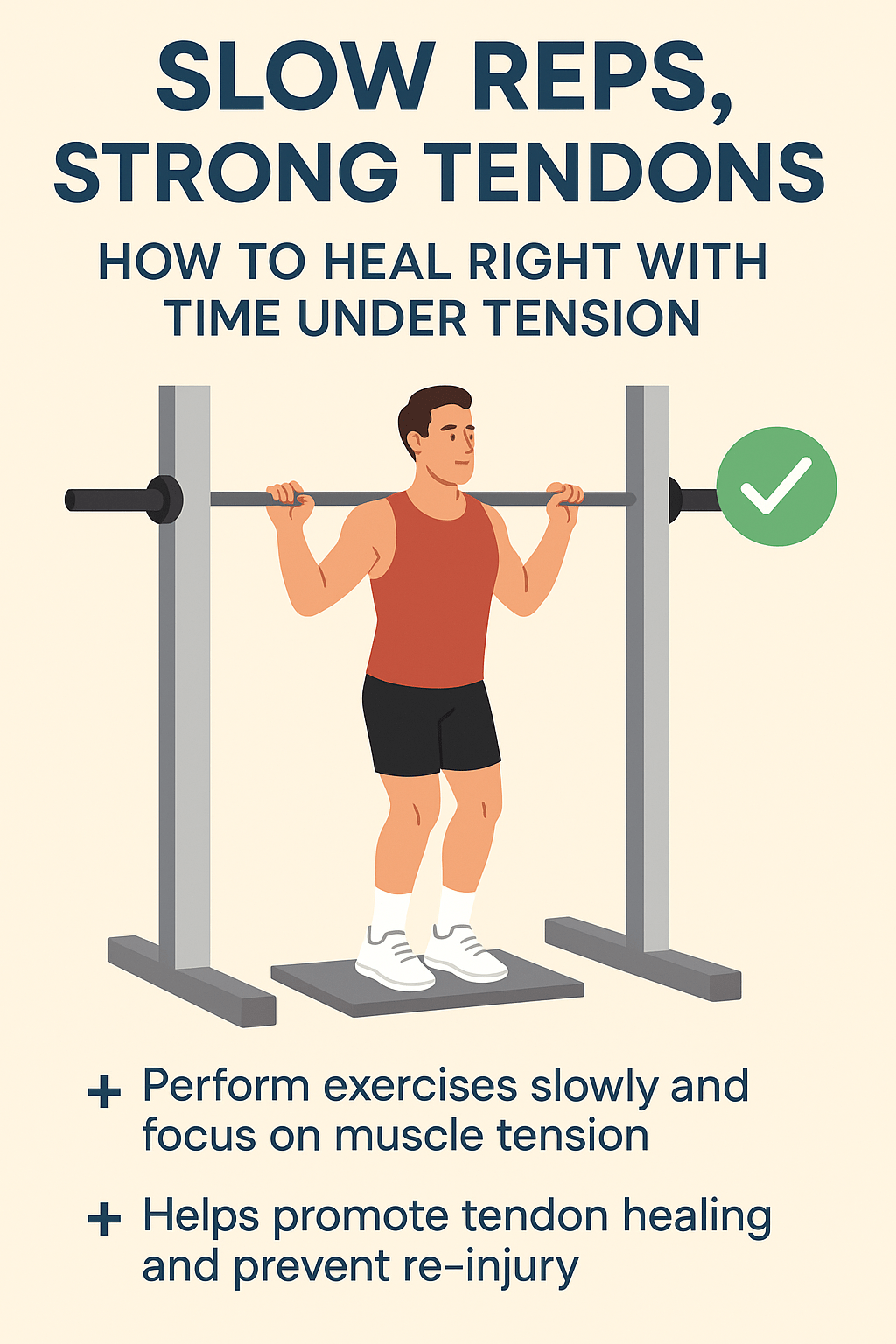
- Time under tension matters: slower, longer-duration loading (e.g. 6-second holds) leads to greater tendon adaptation than fast movements at equal volume.
- Isometric loading may provide superior stiffness adaptation, potentially due to higher mechanical signal density per unit load.
- Overloading can cause ECM microdamage, and insufficient rest between sessions may impair remodeling despite low metabolic demand.
- Tendon hypertrophy is possible with both eccentric and concentric training if mechanical stimulus is sufficient—modality matters less than load structure.
🐇
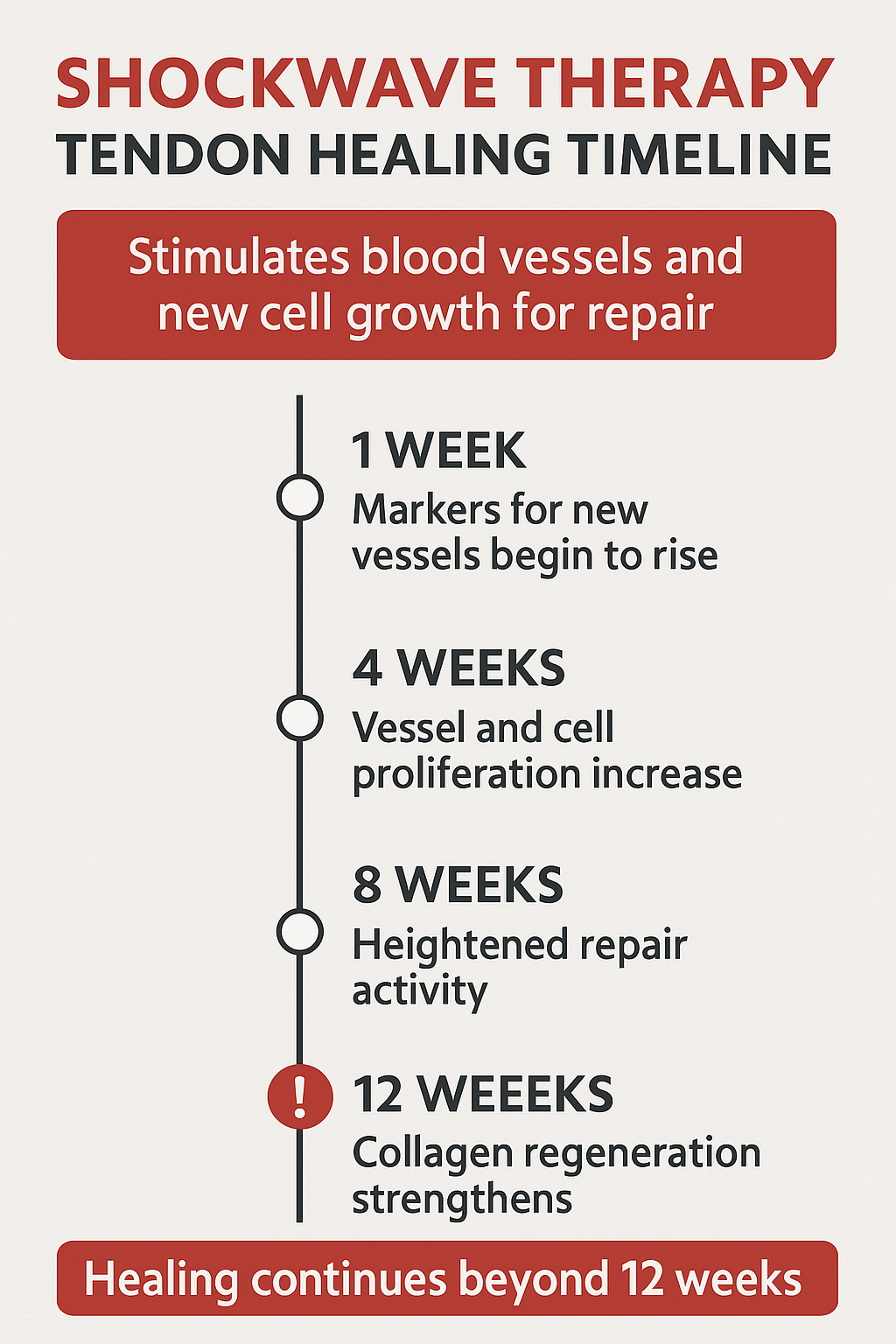
3. Wang et al. (2003) – Shockwave Therapy in Rabbit Tendons
- Focused shockwave therapy stimulated neovascularization at the tendon–bone junction in rabbits, confirmed by histology and angiogenic markers.
- Key molecules eNOS and VEGF increased at 1 week, peaked by week 4–8, and began returning to baseline by week 12.
- PCNA (a cell proliferation marker) rose at 4 weeks and remained elevated through 12 weeks, indicating sustained regenerative activity.
- Neovessel formation started around week 4 and was significantly greater than in controls—lasting through at least week 12.
- Shockwaves induce biological effects in soft tissue, not only mechanical disruption—suggesting molecular healing pathways are activated.
- Tendon regeneration is time-dependent, with the therapeutic window of biological remodeling following shockwave extending over 8–12 weeks
Summary: 6 Core Principles
1. Tendons are Slow Responders
-
Tendons have low cellular activity and blood supply.
-
Core collagen structure is laid down in adolescence and changes very little after age ~17.
-
Only a small outer layer of tendon adapts during adult loading — similar to tree rings.
2. Loading is Essential – but Dose-Dependent
-
Moderate mechanical load increases collagen synthesis, growth factors (e.g. IGF-1, TGF-β), and enzymes like LOX (for collagen cross-linking).
-
However, there’s a sweet spot: too little = degradation; too much = microtrauma.
-
Isometric, concentric, and eccentric loads all stimulate tendon growth — intensity and time under tension matter more than contraction type.
3. Unloading Rapidly Weakens Tendon
-
Immobilization or offloading leads to 80% decrease in collagen synthesis within 2–3 weeks.
-
Mechanical properties (stiffness, strength) decline before any visible atrophy.
-
Even adding growth hormone can only partially offset the effects of disuse.
4. Ageing Reduces Plasticity
-
Age reduces tendon cell numbers and their ability to migrate, proliferate, or synthesize collagen.
-
But much of the decline is due to inactivity, not age per se.
-
Lifelong physical activity helps maintain tendon stiffness and reduces damaging cross-links like AGEs.
5. Tendinopathy = Disorganized, Swollen, Stiff-but-Weak Tendon
-
Chronic tendon pain is linked to:
-
Disorganized collagen fibrils
-
Increased water, GAGs, and blood vessels
-
Rounder, more numerous fibroblasts
-
-
Loading-based rehab (eccentric, isometric, or heavy slow resistance) can remodel this structure — but very slowly.
6. Healing is Incomplete and Prolonged After Injury
-
After rupture or surgery, tendons remain biologically active (e.g. high glucose uptake) for up to a year.
-
Stiffness recovers slowly over 6–12 months.
-
This prolonged activity suggests rehab must be long-term and progressive.Clinician Note — Helen’s Experience (11 Years in Shockwave)
Over the past 11 years, Helen has used both focused and radial shockwave therapy on a wide range of tendon issues — from Achilles and patellar tendons to hamstrings and glutes. In our hands, combining targeted loading with shockwave stimulation accelerates tendon remodeling and creates a more robust recovery. While tricky tendons may take up to a year to fully regain strength, most see steady structural progress within six months when therapy is consistent and individualized.
-